An in depth guide to the link between sugar and cancer and why is it important
There is so much information available online about sugar and cancer that it’s really hard to know what to believe. When you or a loved one have just received a cancer diagnosis you want to learn the facts as quickly as possible and truly understand if cancer patients should avoid sugar.
At the Cancer Coach we consider that there is enough research linking high sugar consumption to poorer prognosis, poorer outcome and poorer quality of life and therefore we recommend keeping sugar consumption to a minimum and will explain why in this in depth guide.
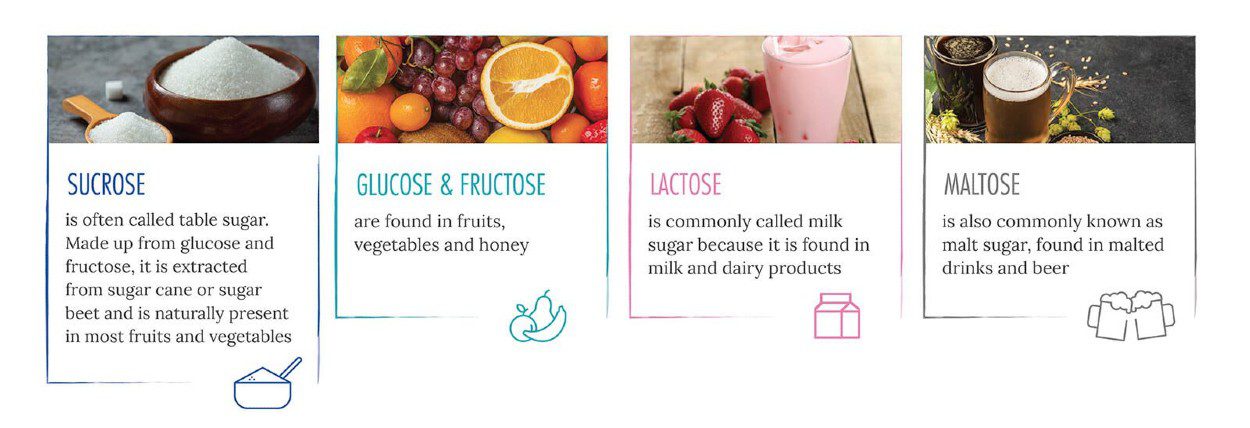
SUGARS are a natural ingredient in human diet. Sugars come in many forms, as single molecules (glucose, fructose), as pairs of molecules (saccharose) or longer chains of molecules (polysaccharides). Together with starches, SUGARS belong to the CARBOHYDRATE family of macronutrients, that our bodies break down into simple sugars in the process of digestion (the works of our digestive system). They are all a source of energy for our cells, with glucose being the most important for the body as it is the “energy source” for our brain. They can be found naturally in fruits and vegetables and added to processed foods and drinks.
What people often refer to as table SUGAR (as in “do you take sugar with your coffee?”) is one of the many types of SUGARS… namely SUCROSE. When we read on a label “no added sugars”, sucrose, or glucose or lactose might be the ones they are referring to.
Source: https://makingsenseofsugar.com/all-about-sugar/what-is-sugar/ consulted on 20/03/2021.
Sugars and their healthy intake are and have been in the spotlight for many years. We are consuming more and more sugar in our diet, if you look at statistics, for the last 40 years, the worldwide sugar consumption per capita has been rising year after year. (2020 has been the first year where consumption has fallen, presumably due to covid restrictions).
In 2015 WHO set up a series of recommendations with respect to free sugar intake[1]:
- Reduced intake of free sugars throughout life (strong recommendation).
- Reducing the intake of free sugars to less than 10% of total energy intake both in adults and children (strong recommendation).
- Suggests a further reduction of the intake of free sugars to below 5% of total energy intake (conditional recommendation).
The European Food Safety Authority (EFSA) was asked to provide scientific advice on added sugars in 2017 and developed a scientific protocol – a detailed plan for the conduct of the assessment[2]. In 2019, ESFA updated the timeline for the release of its scientific advice on dietary sugars due to the high volume of information to be assessed.
This interest in sugars is prevalent worldwide. The reason: an excess of sugar in our bodies poses a significant risk for our health.
Taking all of that into consideration the remainder of this guide will focus on the impact of SUGAR on YOUR health as a cancer patient.
What is the link between sugar and cancer?
Glucose is the basic fuel that powers every single one of our cells. Glucose present in drinks gets absorbed straight into our blood ready for our cells to use. If a starchy food, such as pasta, is our lunch, the enzymes in our saliva and digestive juices break it down into glucose. And if for some reason there is no carbohydrate in our diet, cells can turn fat and protein into glucose as a last resort, because they need glucose to survive.
Cancer is a disease where cells divide with no control, they usually multiply quickly and for that they need a lot of energy. Glucose is their energy, but they can also manage to obtain energy bypassing the use of this sugar. And we cannot forget that cancer cells also make use of a lot of other nutrients too, it is not just sugar they need.
Is sugar bad for cancer patients?
There is indeed a link between a high-sugar diet and cancer risk. And it is very important that you understand what that link is because there is no evidence that following a “sugar-free” diet lowers the risk of getting cancer or boosts the chances of surviving if you are diagnosed.
This can be quite confusing for cancer patients and their carers. Why all the fuss about sugars and cancer if cutting out sugar does not help treat cancer? Why do you receive advice on lowering your sugar intake?
Because there are INDIRECT links between cancer risk and sugar. And these are the ones you need to understand to fully comprehend the unhealthy effect sugar can have in oncology patients.
1st Link: Being Overweight or Obese
Sugar is a highly palatable food that triggers our reward systems due to both caloric input and taste. Taken in excess, sugar can trigger these reward systems too strongly, inducing compulsive eating.
Countless studies have confirmed that consuming foods with a high sugar content on a regular basis drastically increases our risk of gaining weight.
Overweight and obesity are defined as abnormal or excessive fat accumulation (top fat layer under the skin and deeper layer around internal organs known as “visceral or abdominal” fat) that may impair health.
An easy way to determine whether a person is within the obese weight range is to calculate the body mass index (BMI). It is a simple index of weight-for-height that is commonly used to classify overweight and obesity in adults. It is defined as a person’s weight in kilograms divided by the square of his height in meters (kg/m2).
For adults, WHO defines overweight, and obesity as follows:
- overweight is a BMI greater than or equal to 25; and
obesity is a BMI greater than or equal to 30.
Raised BMI is a major risk factor for noncommunicable diseases such as[3]:
- cardiovascular diseases (mainly heart disease and stroke).
- diabetes.
- musculoskeletal disorders and
- some cancers (including endometrial, breast, ovarian, prostate, liver, gallbladder, kidney, and colon).
Overweight and obese women for example have a higher risk of being diagnosed with breast cancer.
We must point out that there are different degrees of association depending on the cancer subtypes, the stage of the vital cycle and the ethnicity of the patient.
The effects of obesity on the risk of breast cancer in premenopausal and postmenopausal women differ based on ER status. In premenopausal women, obesity is associated with a lower risk of ER‐positive breast cancer and a higher risk of TNBC. However, in postmenopausal women, obesity is associated with a markedly higher risk of ER‐positive breast cancer, particularly in nonusers of HT, but with only a modest or no effect on the risk of ER‐negative breast cancer. In contrast, obesity increases the risk of death in both premenopausal and postmenopausal patients with breast cancer. Both biologic factors and undertreatment of obese patients appear to contribute to poor breast cancer outcomes in obesity[4].
Obesity is associated with a higher risk of premenopausal ER‐negative and triple-negative breast cancers (TNBC). On the contrary, most studies report that obesity is associated with lower estrogen receptor (ER)‐positive breast cancer risk before menopause[4].
Obesity consistently associates with higher postmenopausal breast cancer risk in many studies [4]. This association may be limited to ER-positive breast cancers as the risk of ER‐negative breast cancer and TNBC is minimally or inversely associated with obesity after menopause.
Being overweight also increases the risk of recurrence and mortality in women diagnosed with breast cancer
But, when it comes to discussing CANCER risk and obesity, more than just BMI one must consider the deeper fat layer that surrounds your vital organs, the abdominal or visceral fat, which is directly linked to the cancer risk. In vitro studies show that visceral fat tissue can release a protein that can transform a normal cell into a malignant one [5]. There is also evidence that high visceral fat percentage (VAV%) has a negative prognostic impact in endometrial cancer [6].
Adding to that we also know that estrogen production after menopause largely occurs in adipose (fat) tissue, High levels of estrogen can increase your risk of breast cancer and ovarian cancer.
Of course, there are many other factors that lead to weight gain and obesity but sugar is particularly vicious because:
- it is highly addictive and that’s why it is so difficult to limit sugar intake
it tends to increase your appetite,
it is hidden in so many foods.
2nd Link: An increase in blood sugar levels & hormone levels (insulin).
If you consume high amounts of sugar on a regular basis, it can lead to chronically elevated blood sugar levels, known as HYPERGLYCEMIA.
Let us review a few facts about Hyperglycemia:
It is a condition that can lead to type 2 diabetes (T2DM):
Several meta-analyses have found that diabetes represents a risk factor of certain cancers, especially pancreatic, hepatocellular, hepatobiliary, endometrial, breast, and colon.There is also evidence that DM is associated with increased cancer mortality [7]
Recent research shows that HYPERGLYCEMIA also has a negative impact on our DNA: In 2019, a team of researchers found that hyperglycemia, or high levels of glucose in the blood, may induce DNA damage and inhibit DNA repair; It is this impact on the DNA that increases cancer risk [8].
Hyperglycemia promotes INSULIN RESISTANCE. Let me explain a bit what this is:
Carbohydrates from the food you eat are broken down into glucose. As discussed earlier, your body uses glucose as fuel for your muscles, organs, and brain.
But glucose cannot be used as fuel until it enters your cells. That is where insulin comes in. Insulin is a hormone produced by our pancreas, that unlocks cells so that glucose can enter them. Basically, insulin moves sugar from your blood into cells.
When your blood sugar is constantly high, you can develop Insulin resistance meaning that your cells stop responding properly to insulin and can’t use glucose from your blood for energy. To make up for it, your pancreas makes more insulin, it becomes a vicious circle. High levels of insulin, also known as hyperinsulinemia, has been linked to obesity, heart disease and cancer.
What is the link between insulin and cancer?
- Insulin stimulates cell growth, through the interaction with Insulin specific receptors.
- It is known that cancer cells have many more insulin receptors than normal healthy cells [9]. If you have an environment high in sugar where insulin is also increased, it is a more favourable environment for cancer cells to grow.
- Insulin promotes angiogenesis, which is the growth of new blood vessels, meaning that it facilitates the growth of cancer cells, especially in solid tumors because they receive more oxygen supply.
- ngiogenesis also allows cancer cells to potentially travel to other places of the body and create metastasis.
3rd Link: Inflammation [10]
What you eat has a significant impact on the inflammatory state of the body — some foods increase inflammation, while others reduce levels of inflammation.
A diet with high content in sugar creates inflammation in the body, which can lead to chronic inflammation. The mechanism by which this occurs involves our liver. Sugar stimulates the production in the liver of free fatty acids. When the body digests these fatty acids, the resulting molecules can trigger inflammation.
A systematic review from 2018 reported that several studies have linked consuming more dietary sugar — especially from sugary drinks — with chronic inflammation.
People with higher sugar diets have more inflammatory markers in their blood, including a marker called C-reactive protein.
Chronic inflammation can cause DNA damage, which by now we know, leads to cancer.
Studies have also linked chronic inflammation levels to higher risk of breast cancer RECURRENCE [11,12].
4th Link: Gut health
Trillions of bacteria live inside our digestive system. They help digest food, supply essential nutrients, synthesize vitamin K, and promote angiogenesis and enteric nerve function. They fundamentally play an important role in your overall health. They affect everything from your metabolism to your mood to your immune system.
Like a fingerprint, each person’s microbiota is unique: the mix of bacteria in your body is different from everyone else’s mix.
However, research suggests that gut bacteria can be potentially harmful due to the change in their composition (and intrinsic balance) when the gut ecosystem undergoes abnormal changes as a consequence of the use of antibiotics, illness, stress and dietary habits [13]. A diet high in processed foods and added sugars has a negative effect on your gut health as it can decrease the number of good bacteria in your gut.
Unbalance gut microbiota is linked to risk of diabetes, obesity, depression, and certain cancers, especially colon cancer.
What is even more interesting is that recent Studies suggest that our microbiome impacts cancer initiation but also cancer progression. Certain microbes enhance cancer cell fitness by promoting proliferation and protecting cancer cells from the immune system. The International Agency for Cancer Research has designated at least ten microorganisms as carcinogens, one of them being Helicobacter pylori for its link to stomach cancer [14]). Moreover altered gut microbiota is associated with resistance to chemo drugs or immune checkpoint inhibitors (ICIs). Modulating the microbiota via antibiotics, probiotics, faecal microbiota transplant or nanotechnologies may potentiate the antitumor effects of chemo drugs or ICIs [15]
On the bright side of the microbiome, some bacterial species are essential for the antitumor effect of cancer treatment. Cancer patients who have a healthy microbiome seem to respond better to cancer therapies including cancer immunotherapy and seem to have less side effects.
5th Link: Sleep [16]
Sleep plays a major role in our general health and specifically for our immune system. If you do not sleep long enough or do not have good sleep quality, it will negatively affect your immune system and reduce your body’s ability to fight off any disease.
Too much sugar leads to a tendency to eat later in the day because blood sugar levels are zigzagging out of control. That adversely affects sleep, and your disrupted sleep will, in turn, produce an even greater craving for sugar the next day. The vicious circle is ongoing. A study conducted in 2016 [17] showed that low fiber and high saturated fat and sugar intake is associated with lighter, less restorative sleep with more arousals. Sugar uses up a lot of magnesium, which you need for sleep,
Being Sleep deprived also exacerbates side effects of cancer treatment, and intensifies the feeling of pain.
The Cancer Coach can review your diet with you and not only identify areas of improvement but give you a customised plan to help you implement these changes along with recipes, meal plans and regular 1-1 support.
Book a Free Cancer Consultation
Bibliography:
[1] WHO. WHO calls on countries to reduce sugars intake among adults and children. (15th March 2015). Accessed on March 31st, 2021: https://www.who.int/news/item/04-03-2015-who-calls-on-countries-to-reduce-sugars-intake-among-adults-and-children
[2] European Food Safety Authority. EFSA to give advice on the intake of sugar added to food. (23rd March 2017). Accessed on March 31st, 2021: https://www.efsa.europa.eu/en/press/news/170323-0
[3] WHO. Obesity and overweight (1st April 2020). Accessed on March 31st, 2021 https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
[4] Klepsland Mauland K et al. (2017) High visceral fat percentage is associated with poor outcome in endometrial cancer. Oncotarget. Vol. 8 (62): 105184-105195.
[5] Chakraborty D et al. (2017) Fibroblast growth factor receptor is a mechanistic link between visceral adiposity and cancer. Oncogene. 36(48):6668-6679.
[6] Picón-Ruiz M et al. (2017) Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention CA Cancer J Clin; 67(5): 378–397. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5591063/#
[7] Suh S, Kim KW. (2019) Diabetes and Cancer: Cancer Should Be Screened in Routine Diabetes Assessment. Diabetes Metab J.43(6):733-743.
[8] Termini J: American Chemical Society Fall 2019 National Meeting & Exposition. Abstract TOXI-4. Presented August 25, 2019. Accessible at https://plan.core-apps.com/acs_sd2019/abstract/d5901b87-9d3d-4061-abc5-e96df83ef123
[9] Vigneri R, Goldfine ID, Frittitta L. Insulin, insulin receptors, and cancer. J Endocrinol Invest. 2016 Dec;39(12):1365-1376. doi: 10.1007/s40618-016-0508-7. Epub 2016 Jul 1. PMID: 27368923.
[10] Does sugar cause inflammation in the body? Medical News Today (September 19, 2019). Accessed on March 31st, 2021 from https://www.medicalnewstoday.com/articles/326386.
[11] Tobias DK, Akinkuolie AO, Chandler PD, Lawler PR, Manson JE, Buring JE, Ridker PM, Wang L, Lee IM, Mora S. Markers of Inflammation and Incident Breast Cancer Risk in the Women’s Health Study. Am J Epidemiol. 2018 Apr 1;187(4):705-716.
[12] Steve W. Cole, Ph.D.1. Chronic inflammation and breast cancer recurrence J Clin Oncol. 2009 July 20; 27(21): 3418–3419
[13] Yu-Jie Zhang et al. (2015) Impacts of Gut Bacteria on Human Health and Diseases. Int. J. Mol. Sci. 16, 7493-7519.
[14] Whisner, C.M., Athena Aktipis, C. (2019) The Role of the Microbiome in Cancer Initiation and Progression: How Microbes and Cancer Cells Utilize Excess Energy and Promote One Another’s Growth. Curr Nutr Rep 8, 42–51.
[15] Cheng WY, Wu C, Yu J (2020) The role of gut microbiota in cancer treatment: friend or foe? Gut;69:1867-1876.
[16] Stephen Moss. The alarming truth about how sugar ruins your sleep. The Guardian (Sun 12 Jan 2020)
[17] Marie-Pierre St-Onge, et al. Fiber and saturated fat are associated with sleep arousals and slow wake sleep. (2016) Journal of Clinical Sleep Medicine 12, (1):19-24.